Star Tribune graphic by Michael Godfrey
The Ulcer "bug"
Health & Fitness – Health Notebook
Star Tribune – Thursday,
April 17, 1997
[ Note: Australian gastroenterologist Barry Marshall, M.D. and pathologist J. Robbin Warren proposed their theory for the bacterial cause of peptic ulcers in 1983. The bacterial cause of gastric ulcers in pigs was known in 1952. ]
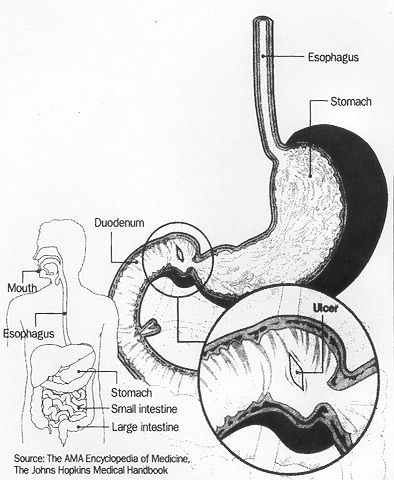
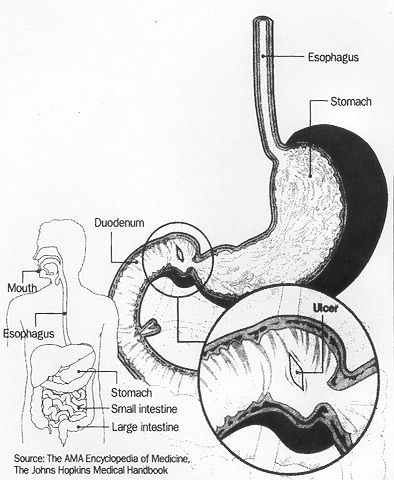
If you're one of the 5 million Americans with duodenal ulcers, you aren't, as
you may believe, the victim of excess stomach acid, too much coffee, fried
food or a cement–headed boss.
You are most likely the victim of a spiral–shaped bacteria,
Helicobacter pylori.
The bug lives in the lining of your stomach, and washes down into the upper
bulb of the duodenum, the first part of the small intestine where most ulcers
occur. There it gnaws at the lining, initiating a painful ulcer, and somehow
signals the stomach to produce more hydrochloric acid and more pepsin, a
digestive enzyme. The pain of an ulcer can be relieved by eating.
Half of adults older than 60 have H. pylori in their bodies, but only a small
percent of them develop ulcers. Among younger people, only 5 to 10 percent
have H. pylori infections, and far fewer have ulcers.
It is not known why some people develop ulcers from the bug and others don't.
One bad thing: H. pylori is hard to reach in the lining, so the antibiotics have to be taken daily for two weeks even though the painful symptoms of ulcers disappear fairly soon after treatment starts.
Most of the other 10 percent of ulcers occur in people taking large doses of anti-inflammatory drugs, such as aspirin and ibuprofen, for extended periods. The drugs tend to erode the wall of the intestine.
Those ulcers almost always clear up when people take stomach-soothing drugs such as Zantac and stop taking aspirin or ibuprofen.
They also thought that stress caused ulcers. Some thought there was an ulcer personality, people who were harried or worried too much.
"It turns out," said Dr. Robert Ganz, a Minneapolis gastroenterologist, "that diet has absolutely nothing to do with ulcers and that ulcers are much more common in people in lower socioeconomic levels than in people in upper socioeconomic levels. Alcohol has nothing to do with ulcers. Smoking probably has nothing to do with it either."
He said it is only a coincidence that both smoking and ulcers are more common among poor people than among the middle–class.
Bland diet and relaxation as treatment were replaced by a more effective, rational method – antacids to neutralize or suppress stomach acid.
"When Zantac [and other acid-suppressing drugs] came along, it almost wiped out ulcer surgery, " Ganz said.
The reason is simple, according to Dr. John Allen, another Minneapolis gastroenterologist. H. pylori is still alive and well in the lining of the stomach, he said.
The saga of H. pylori and ulcers began in 1982 when two Australian researchers, Drs. Barry Marshall and Robin Warren, noticed H. pylori in the lining of the stomach of people with gastritis, inflammations which include peptic ulcers.
To prove that H. pylori wasn't just an innocent bystander, Marshall swallowed a teaspoonful of culture containing H. pylori. He developed hunger upon awakening, irritability and bad breath, all symptoms of gastritis.
Marshall and Warren subsequently established that H. pylori infection causes ulcers in the stomach and the duodenum. It turned out that the bug seemed to cause about half of stomach ulcers, and 90 percent of the much more common duodenal ulcers.
In the early 1990s some gastroenterologists started prescribing antibiotics, usually along with other antiulcer drugs, wiping out both the ulcers and the infections, Allen said.
Now doctors are worried that ulcers may make a comeback because some people fail to take their prescriptions as directed, stopping when the symptoms disappear, but before the bug has been wiped out.
That can allow some live bacteria in the stomach to return stronger than ever and resistant to antibiotics, Allen said.
The most common symptom of an ulcer is a gnawing or burning pain in the abdomen between the navel and the lower part of the breastbone. It most often occurs between meals or in the early morning and can last from a few minutes to a few hours. It usually is relieved by eating food or antacids.
Because the symptoms can be produced by something else, doctors usually have to use X–rays or an examination through a flexible, lighted tube to make the diagnosis.
"There will be a vaccine coming," Allen said. "People are working on it right now."
The Ulcer "bug"
Your Health —
Star Tribune
Personl Health — Sunday, June 29, 1997
Helicobacter pylori, now emerging as the most likely culprit in ulcers, is difficult to diagnose and treatment often requires a combination of antibiotics and other medications to beat it.
Could a person catch ulcers from a housefly? As preposterous as that might seem, it could happen, at least indirectly.
About 90 percent of ulcers are now known to be caused by a slender, spiral–shaped bacterium, Helicobacter pylori, or H. pylori. The resilient organism, found in the stomachs of one fourth of American adults, is believed to spread from person to person by food or water contaminated by fecal matter.
Microbiologists at St. Elizabeth's Medical Center in Boston recently demonstrated that the common housefly can become a reservoir of H. pylori, carrying the organism on its skin and in its intestinal tract and passing the bacterium on in its excretions.
One does not have to be a scientist to envision a likely mode of transmission. Houseflies lay eggs, develop and feed on excrement — human or otherwise — then often land on unprotected food, where they might deposit the troublesome organism and pass it along to an unsuspecting consumer.
If that mode of transmission is correct, it would partly explain why H. pylori infection is most common in poor countries. Indoor plumbing, refrigeration and modern sanitation are often lacking, and H. pylori infection is nearly universal.
A Common Bug
How H. pylori is transmitted is only one of several unsolved mysteries about a bacterium that should become as familiar to people as E. coli, salmonella and pneumococcus. For one thing, scientists are still not sure exactly how H. pylori causes an ulcer, although they know how it is able to survive and flourish in the hostile acid environment of the stomach.
But the most pressing question is why, when so many people harbor the organism, often for their entire lives, do only a few develop ulcers? And why do even fewer develop two forms of stomach cancer that are also attributed to H. pylori infection? One strain of the organism has a gene that renders it more virulent than other strains. But is that the whole answer? Are human factors also involved?
There is no simple way to predict who is likely to get sick from an H. pylori infection, so people could be treated to eliminate the organism before illness strikes.
Does Stress Play a Role?
Although discovery of H. pylori has prompted experts to discount stress as a cause of ulcers, might stress–induced changes in body chemistry explain why some people are susceptible and others are resistant to ulcers caused by the bacterium?
Then there is the treatment dilemma: the inability so far to find a simple way to cure an H. pylori infection. Three or four drugs taken simultaneously are best able to knock out the organism, but the more complicated, costly and unpleasant the treatment regimen, the less likely people are to follow it and be cured.
Thanks to the discovery of H. pylori 15 years ago by Australian scientists Barry Marshall and J. Robin Warren, most people, who develop the symptoms of an ulcer can be spared the constant threat of recurrence once they are treated with appropriate antibiotics.
They no longer have to gobble antacids forever or live on a bland diet, avoiding all spices, alcohol and coffee to squelch the pain that arises in the upper abdomen whenever their stomachs are empty or they consume irritating foods. And although reducing stress is always a good idea, ulcer or no ulcer, relaxation therapy is not essential to keeping the distressing ailment at bay.
There are several ways to diagnose an H. pylori infection. The simplest and least expensive is a blood test that can detect antibodies to H. pylori. But the test cannot distinguish between a current active infection and a past one. A second more expensive blood test may be needed to be certain of the diagnosis.
A Breath Test
Amore costly but also more precise method is the recently approved urea breath test. The patient consumes a small amount of urea that has a special form of carbon. If H. pylori bacteria are present in the stomach, a short while later the patient will exhale carbon dioxide that has the special carbon.
With the tests doctors usually can avoid having to insert a fiber–optic tube into the stomach to examine the stomach lining and to take a tissue sample to test for H. pylori. Although it is the most accurate test, it is also the most expensive and discomforting, and it must be administered by a specialist in gastroenterology.
A test not yet approved relies on detecting the genes of the bacteria in dental plaque or stool samples. It is quick and painless, and it can identify the particular strain of the organism.
Experts recommend testing anyone who has a new or recurrent stomach or duodenal ulcer, including those who regularly take nonsteroidal anti–inflammatory drugs such as ibuprofen and aspirin, which are known produce ulcers in some people But people with chronic acid digestion need not be tested because treatment to eradicate H. pylori infection, if found, has not been shown to relieve the symptoms.
No Easy Treatment
Anyone with an active ulcer or a healed ulcer who is found to harbor H. pylori should be treated to eradicate the organism. But the bacterium does not go down without a good fight. No one drug is fully effective, and the organism readily develops resistance to antibiotics. Thus is important to hit it hard and effectively with the first round of treatment.
There are several treatment options, none of them easy or pleasant. All involve a two–week regimen that combines one or two antibiotics and a substance that coats stomach lesions or a substance that inhibits secretion of stomach acid or both. The cost of medication ranges from $30 to $200.
Two four–drug regimens that include the antibiotics metronidazole and tetracycline with bismuth ( Pepto–Bismol ), which coats the stomach, and omeprazole ( Prilosec ), an acid inhibitor, are the most effective, eradicating the organism in 95 percent of cases.
Although the drugs cost more than $100, and the treatment is complex, it pays to follow it closely if you want to be cured. Side effects, which may include diarrhea, taste disturbances, nausea and black stools, disappear when the treatment is completed.
— Jane Brody writes about health and medicine for the New York Times.
Ulcer Cause: The National Institutes of Health has confirmed that peptic ulcers can be caused by a bacterium and drug therapy can prevent a recurrence in 90% of cases. An NIH panel stated Wednesday that Helicobacter pylori plays a significant role in causing peptic ulcer, which can be cured with a combination of bismuth, tetracycline and metronidazole. The panel also said that H. pylori is linked to gastric cancer but found no data to show preventing or treating infection reduces the cancer risk.
Look Good, Feel Good
Mom Was Right ... Eat your veggies !!!
A recent study shows that broccoli and broccoli sprouts contain a chemical that kills H. pylori — the bacteria responsible for most gastric ulcers and stomach cancers.
Dr. Paul Talalay, a researcher at John Hopkins, had previously reported that a chemical in cruciferous vegetables, especially broccoli, called sulforaphane is an effective anticancer agent. Scientists are working to develop varieties of broccoli with higher levels of the chemical. Study findings are reported in a recent issue of the Proceedings of the National Academy of Sciences.
[ Cruciferous – any plant of the mustard family, including the cabages, cresses, etc. ]
Journal of the American College of Nutrition 2003:22(4), pp 283-289
Simon JA, Hudes ES, Perez-Perez GI.
Relation of serum ascorbic acid to heliobacter pylori serology in U.S. adults:
the Third National Health and Nutrition Examination Survey.
http://www.jacn.org
Evidence suggests that low levels of ascorbic acid in the blood may increase the risk of several gastrointestinal disorders, including peptic ulcers and gastric cancer. Chronic infection with the Heliobacter pylori bacteria - particularly a strain known as cagA - may also contribute to gastric cancer and peptic ulcers. Some research suggests that H. pylori and ascorbic acid concentrations are not related, but these studies had small sample sizes. Prior to the current study, no large-scale studies had examined the relationship between blood ascorbic and H. pylori levels.
Researchers tested blood samples of 6,746 adults enrolled in the Third National Health and Nutrition Examination Survey. Of the test subjects, 32% tested positive for H. pylori; of those, 54% had the cagA strain. The gender, percentage of current cigarette smokers and self-reported use of NSAIDs were similar among those who tested negative.
Analysis of the blood samples revealed that ascorbic acid rates were inversely related to the prevalence of H. pylori. In patients whose serum ascorbic levels were 0.35 milligrams or less, the infection rate with H. pylori was 37.2%. For patients with serum ascorbic levels of 0.36 or higher, the infection rate dropped to 30.8 percent, even after adjusting for variables such as age, race, body mass index, physical activity level, use of aspirin or NSAIDs, and cigarette smoking. This finding was statistically significant. In Caucasian subjects, the analysis found that a 0.5 milligram increase in blood ascorbic levels was associated with a 31% decrease in the prevalence of the cagA strain of H. pylori.
The researchers concluded: "Serum ascorbic acid is significantly correlated with seropositivity to both H. pylori and to the pathogenic cagA-positive strain of H. pylori among white Americans. To our knowledge, this report is the first population-based study of Americans to report such associations. If these findings are confirmed by other investigators and are linked causally, higher intakes of ascorbic acid may be a protective factor in the prevention of H. pylori infection."
Friendly Bacteria, Almost Completely Eliminates Salmonella in Chickens
Naturally Occurring, Symbiotic, Probiotic Micro-organisms
Introduction to Effective Microorganisms
The Tortoise Shell "Science of Health" Newsletter
Friendly Bacteria inhibit the growth of other strains that are not so friendly to animals.
It is the waste products that bacteria create and release that do much of the damage.
Taking an Anitbiotic to Treat a Disease, Kills the Friendly Bacteria Also !
Inorder to Maintain Optimum Health, the friendly bacteria need to be replaced after treatment.
"Active Culture Yogurt" is one very good and inexpensive source of friendly bacteria.
— Putting an End to Disease on Our Planet —